Fundamentally our story began with a culture shock.
1999 – I emigrated from Trinidad and Tobago as part of the international recruitment drive to bolster the National Health Service (NHS) nursing workforce. I was one among thousands of nurses who came to the UK in 1999, desperately needed by the NHS, but largely unwelcomed by indigenous nurses and the British public. As fate would have it, my first job was at a small Community Hospital in Teddington which provided Intermediate Care and Rehabilitation for adults 65 years and over. Within a few months, the segregation of health and nursing care of adults at the chronological age of 65+ utterly confused me. My cultural and professional nursing education taught me that people were deemed adults from 18 years until death. It was a shock to realise that in the NHS adulthood, particularly later adulthood, would be characterised by different models, discrimination, different outcomes, and priorities.
2004 – Over the years my confusion evolved into disquiet and discomfort with the notion. By 2004 I had progressed from an overseas staff nurse D grade to Clinical Ward Manager of a 60-bed Intermediate Care Unit at a Health and Care Centre in Brent. I had responsibility for leading and managing the clinical care and discharge planning for thousands of adults, many of whom the multi-disciplinary team (MDT) appeared convinced that 24-hour care was needed and that it could only be effectively provided in a care home or residential home setting. I was part of the decision-making process, but I was never quite comfortable with discharging people to residential and care homes for issues such as ‘acopia’ (being unable to carry out activities of daily living such as cleaning, cooking, and hygiene independently), loneliness as a result of childlessness, or children living far away or loss of lifelong friends, amputations, and consecutive falls. I saw the potential for them to remain in their own homes, but the drivers were always to “free up the bed”, or “he/she was no longer safe at home”, or “it was in the patient’s best interest”, or “they would be with other people their age”.
2007 – During an MDT meeting in 2007, the daughter of a gentleman who was an in-patient at the time, and her husband, were trying to convince her father, who had fallen several times at home, that they had jobs and a life to live and that a care home was the “best place” for him. He sat in silence and listened with tears in his eyes. At one point while the discussion about his future was taking place he leaned over to me and quietly whispered “Sister, if you let them put me in a care home then you condemn me to a life of celibacy”. It was a pivotal moment in my life and career. It changed everything; my philosophy of nursing, how I saw the adults I served, and how much my and the work of others discriminated against adults based on age and medical/social needs. At that time the term ‘ageism’ was not in my vocabulary or narrative. That gentleman and what he said shook me to the core, and I have not forgotten him to this day. He had planted the seed for what was to become my life’s mission and my cause.
2008 – I joined the Technology Strategy Board (TSB), which was rebranded in 2010 as Innovate UK, which then merged with the Research Councils and is now known as UKRI/Innovate UK. My role was that of Lead Specialist on the Assisted Living Innovation Platform (ALIP) and the remit was to develop and deliver business-led innovation challenges to support the NHS to meet the “health care burden’ of Britain’s ageing population. The focus was on supporting the NHS to meet its cost reduction targets and the challenges of the “tsunami” of older people on society and the health service.
2012 – 2015 – As the ALIP was nearing completion of its five-year programme plan, the question was what next? I seized the opportunity to tackle what I felt was a social problem and an archaic model of health and social care, the institutional model of long-term care. I had been a silent witness to the guilt, heartbreak and separation of too many sons, daughters, fathers, mothers, brothers, sisters, grandsons and granddaughters. It didn’t take much to convince Dr David Bott, then Director of Innovation Platforms, that this was a societal challenge of monumental proportions; one that no other country had tackled before or even saw as an innovation agenda. My argument was that there was a dearth of innovation, the potential to unlock new markets, improve quality of life, and create new sustainable health and social care models to reduce impact and cost to the NHS. David recognised the depth and long-term nature of such an endeavour and paved the way for the Long-Term Care Revolution SBRI Sandpit Challenge and the Long-Term Care Revolution SBRI National Grand Challenge to be funded to the tune of £7.8 million.

2016 – In September 2016 I departed Innovate UK and set up my consultancy Marshall-Cyrus and Associates Ltd to support entrepreneurs, micro-businesses, SMEs, and large companies with sector expertise. To maintain my nursing registration I was required to demonstrate hours of clinical practice so I signed up with a nursing agency and returned to clinical practice part-time. My first appointment was at a care home with an outstanding CQC rating. What I encountered over the 48 hours I worked there left me devastated and in a state of utter despair for several days. Over the next 2 years, I experienced and saw the unimaginable. Raising concerns with the relevant authorities met with calls to the nursing agency requesting they no longer send me and inaction by the Care Quality Commission (CQC).
2017 – 2019 – I can only describe this period as one of great emotional and psychological suffering. I confided in a close friend, my career coach for several years, about the things I had seen, the closed cultures, what happened to people who raised concerns or challenged the unsavoury practices, and how managers bullied and harassed staff with impunity. On some of our calls, I would cry inconsolably. I was wracked with guilt that I was so helpless to do anything to meaningfully alleviate the suffering and loss of humanity I witnessed on every single shift. On one such day, he stated “You need to gather a group of people who are not afraid to put their heads above the parapet and say what you are saying. You need a tribe, Jackie”

2020 – 2021 -In April 2020, I convened a group of seven experts in the ageing and social care domains from across the UK (including 3 from Wales) who committed to openly challenge the status quo with me. My first task was to reveal the reality as opposed to the facade of institutional care and organisations which provided care using this model. It was necessary to get them to understand what I and other dedicated healthcare workers in the sector experienced under the cloak of secrecy, closed cultures, and cultures of fear. I knew despite my skill at influencing and impassioning, I did not have the words to convince, so I showed them. It took twenty minutes. I recall the deathly silence that followed, the horrified expressions and the tears streaming down a few faces. I had my Tribe.



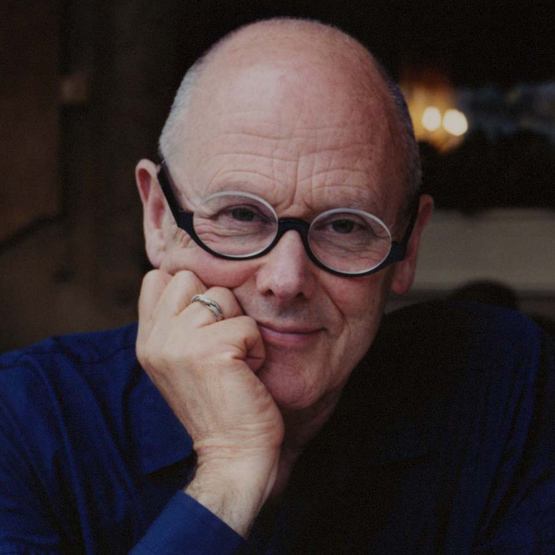


2022 – Between 2021 to December 2022 the Tribe worked relentlessly to break down the magnitude of the challenge. We needed to eat the elephant one bite at a time. We decided that we needed to create a legal entity to deliver the vision. Unexpectedly, our biggest challenge was agreeing a name for the legal entity. Michael Wolff is one of the UK’s most renowned design gurus and we put it to him. He came back with “Jackie”. I rebelled! We all did except for one. After six months of working sessions, it came down to “Jackie’s Revolution”. I rebelled again! This time I was out-voted and for many months studiously reassured stakeholders that I was not the one responsible for the name and that I was not a narcissist. Jackie’s Revolution Community Interest Company (CIC) was incorporated on the 15th July 2022. That year we created the Jackie’s Revolution website with a powerful call-to-arms video and dedicated to campaigning for others to join the revolution. We are truly grateful to Josh Cyrus for the creation of our website and logo. Josh continues to provide IT support gratis to the present day.


2023 – I said there were seven members of my Tribe. Lorraine Morgan was the seventh. Our story would not be what it is so far without her belief, commitment, expertise, skills, experience, and shared vision. What I lack in tenacity, perseverance, and networking skills, Lorraine has in bucketloads. We started on the long and winding road for over a year that seemed to be leading to nowhere. We’ve spoken to key stakeholders, policymakers and funders, all of whom applauded our vision and ambition, confirmed the unsustainability of the institutional, and unfitness for purpose, but were restricted by funding mechanisms all targeted to investing in technological C&D. Without exception stakeholders affirmed a system change was needed, but no organisation was prepared to fund even the first steps to systems innovation. That was until we came across a most unlikely organisation that enthusiastically supported our ambition. In March 2023 the National Lottery Community Fund Wales “Awards For All” funded us to the tune of £10K. We will always be grateful to them for their foresight and vision in supporting us to make the first step on this audacious journey.

2024 – We now have three (3) Directors and an Advisor making up the Senior Management team. Mrs Andrea Nicholas-Jones became our third Director at the end of 2023 and we are thankful to Professor Malcolm Prowle for supporting us with his vast economic management expertise. We have secured a second round of funding from Gwent’s Research and Innovation Initiative and will be delivering more events to help us map what people of the Baby Boom, Millenials, and Generation X want in their advanced years. This includes the Later Life Survey to be found on our website. We are currently exploring collaborations with Welsh Universities, Housing Associations and other key stakeholders. Our journey continues. Despite being a full-time Senior Lecturer at the University of Worcester and Lorraine’s various commitments, including Chair of the Gwent Citizen Panel, we will be relentless in our pursuit of new ways of living out our years other than in institutions. Why? Because growing older should not cost you what it means to be human.


